As I get prepared for my 2-year follow-up MRA this Friday, I was curious to see just how many angiograms and MRA/MRI’s my brain has had since 2006. Thankfully, I was able to get a pretty good handle on that number by simply searching this blog. I was surprised by the number…but not really.
CEREBRAL ANGIOGRAMS
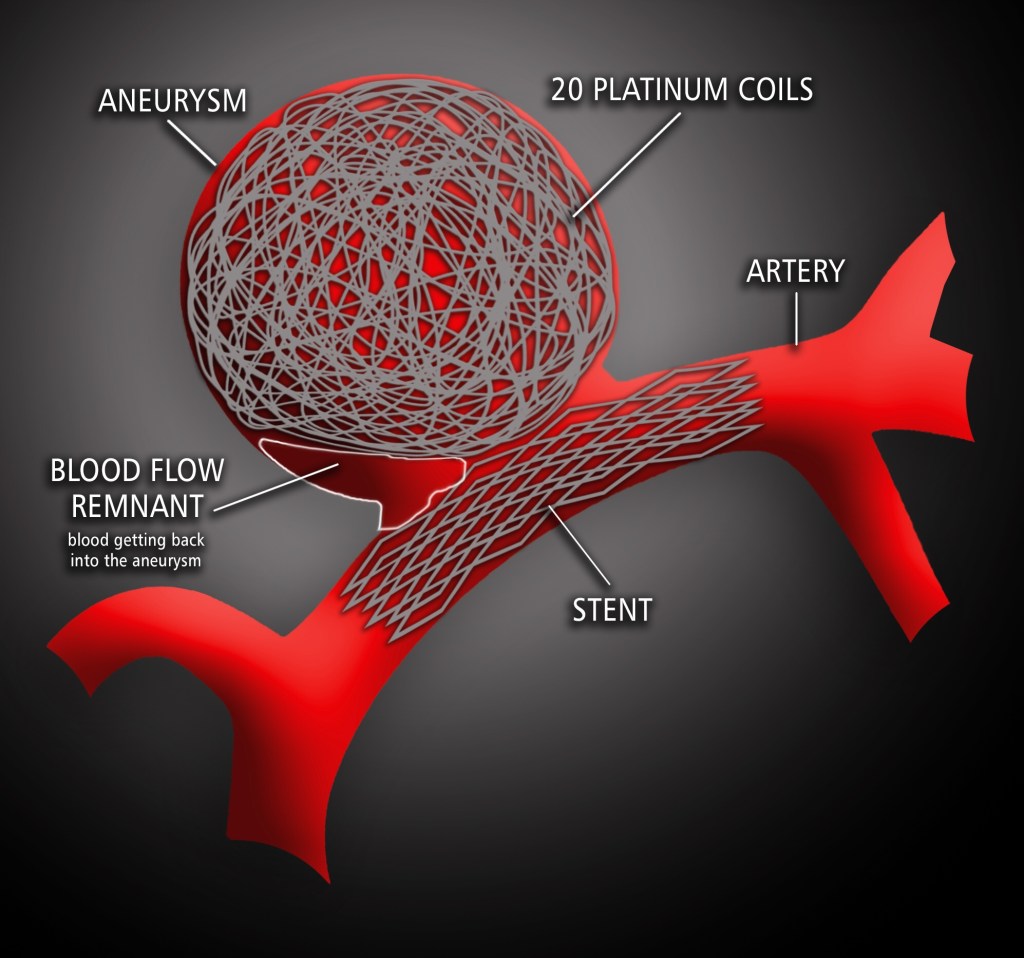
I have had NINE cerebral angiograms which include three treatments that are performed using this same process: my initial coiling, then my stent placement, and recoiling were all performed using angiography.
A Cerebral angiography provides x-ray images of blood vessels in and around the brain, showing abnormalities like brain aneurysms.

PHOTO: John Hopkins Medicine
Typically a catheter is inserted into the femoral artery in the groin and threaded through the circulatory system to the carotid artery where contrast die is injected. A series of images are taken as the contrast agent spreads through the brain’s arterial system, then a second series as it reaches the venous system.
MRA/MRI
I have also had SEVEN MRA/MRI’s. Magnetic resonance angiography–also called a magnetic resonance angiogram or MRA–is a type of MRI that looks specifically at the body’s blood vessels. Unlike an angiogram, which requires inserting a catheter into the body, magnetic resonance angiography is a far less invasive and less painful test.

PHOTO: My brain bling via MRA imaging.
The frequency and type of follow-up procedures I receive hinge on the previous scan showed and what procedure was provided. We’re hoping I can continue just getting MRA’s, but if something unusual shows up, more angiograms may be needed. Angiograms are more invasive and risky, but they are the gold standard for getting the clearest images of my blood vessels.
I am blessed to have had such a great neuro team here in Maine and terrific health insurance coverage through work.
Here’s to more scanxiety.