I’m seriously hoping this is my last angiogram for awhile. I’ve seen that angriography suite far too often the last several years. However, it’s the best way to see what’s really going on with my pesky vascular system.
As stated in my previous blog entry, this angiogram was to determine if there were any changes to my original 11mm brain aneurysm from last year when it was discovered more blood was starting to creep back into the neck of the aneurysm. Obviously, the 20 coils and the one stent weren’t doing the best job they could be, but I’m still here.
Since there was a chance I’d be staying overnight, I had to go to admissions first and check in, then we went straight to the radiology department. They were quite busy today, although I reminded myself I’m usually scheduled for much earlier appointments. This is the first time I’ve had an afternoon appointment and I was VERY hungry and thirsty after not having anything to eat or drink since midnight the night before.
Upon entering radiology, Dave and I were greeted from a distance by nurse John, who we usually see when we arrive there. It’s a mixed blessing when you’ve visited a place so often you become so familiar with the staff of a hospital. John told my attending nurse that I didn’t need any instruction because I knew exactly what I was supposed to do in here. LOL Yes…pretty true.
The IV was hooked up, more questions were asked, and more instruction was given. We were most curious about the balloon occlusion test and what that entailed.
The BOT is a little more risky and it would also require another port and catheter into my other arm where something would be injected to bring my blood pressure down during the test. I wasn’t looking forward to TWO catheters. Dr. Ecker explained the risks and why they’d keep me over night as more of a precaution. If I was doing great after the whole thing I could potentially go home and not have to stay.
I said my good-bye’s to Dave and was wheeled into the radiology angiography suite. As usual, the teams assembled for every single angiogram I’ve had at Maine Medical Center are top notch and always make me feel comfortable and at ease. Even though I’ve gone through many of these, it’s still a nervous time.
They allowed me to request a music station on their Pandora internet radio that was piped into the suite. I chose 80’s Throwback music. As the doctor walked in he said the music was a step up from the morning sessions. I said “You’re welcome”.
So enough of the pleasantries and on to the drugs, please! I’ve always had some pretty good pain when the catheter in my groin is inserted and I always request a little extra something special. Thankfully, they complied and it wasn’t too bad. They also inserted the IV into my left arm to prepare for a catheter for the balloon occlusion test. That was a little painful as well, but it didn’t last long.
I know many people don’t understand why my groin hurts after having X-rays done on my brain. Aren’t they a tad far away from each other? Well, yes, but inserting a dye into that area gives a direct flight into the brain via one of the main cerebral arteries. I’m not sure why it’s going from the groin and not up higher on the body, such as the neck or chest, but it works, so I’m not going to question it.
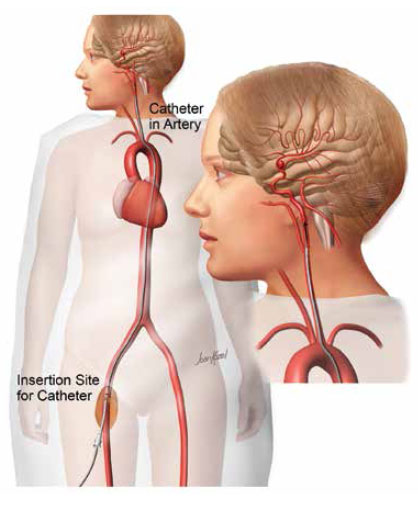
During the angiogram, they take a series of images of the arteries then inject a dye to see exactly where the blood is flowing and take another series of X-rays. When the dye is injected I see a series of small horizontal lightning strikes behind my left eye. It’s brief, but weird. I keep my eyes closed during the whole thing, mainly because I’m dopey and can’t see anything without my glasses anyway, but because there is usually part of the machine directly above my head and there isn’t anything to see anyway.
After the initial angiogram, Dr. Ecker compared images taken last year at this time with the ones he just took. He was able to pull them up on the screen side-by-side, then even overlap them. He indicated there was absolutely NO change from last year, which was great news. Then he was questioning if we should even go ahead with the balloon occlusion test at that point since nothing had changed.
The main reason we were going to do the balloon occlusion test in the first place was to see if my vascular setup could even handle such a reversal of blood flow should a I NEED to have something dramatic done to prevent more blood from getting into the brain aneurysm.
Since there didn’t appear to be any immediate need for that, based on this angiogram, we both decided to forgo the BOT this time. I was okay with that. I wasn’t looking forward to more pain, or an overnight stay. However, a part of me was disappointed we just didn’t do it and get it over with now so we’ll know down the road.
Because they had expected to do a lot more, the large team assembled for this big event wasn’t really needed now and the last thing remaining in the radiology suite was the dreaded “plug”, or Angio-Seal™. The angio-seal is a small device that basically closes up the puncture site in the groin. However, since he used a larger catheter for today’s procedure, that larger plug was needed. It can be quite painful, mainly because I’ve been “poked so many times” as he said. Lucky me!
Why, yes…it WAS painful and they had to tell me to calm down, relax, and keep my leg down. I did. Still hurt. LOL The UPSIDE of using the closure device is that I only have to lay flat in recovery for two hours, not four or more hours if they were simply to apply preasure to the site for 15 minutes. The angio-seal allows the bleeding to stop much more rapidly and a quicker discharge from the hospital So, that’s the trade off for the pain.

The seal is comprised of three absorbable components: a small anchor, collagen, and a suture. The doctor guides the anchor through the hole created during the procedure where it is drawn in against the wall of the artery and the suture and collegian compact to create a secure seal over the entry point in the groin. All three components dissolve and are absorbed into my body in about 90 days. I’ll have an odd bump there for awhile, but the pain should ease after a few days.
The recovery in the radiology department is always long, but it seemed more so this time because they kind of forgot to offer me any food or water. It wasn’t until Dave asked them about an hour into my stay that I got a sandwich and some water. That’s highly unlike that crew and I was a little surprised.
Once they had me up on my feet for a short walking test and determined I wasn’t dizzy or unstable, I was discharged and walked out on my own. The only stop on the way home was at McDonalds for a shamrock shake! ‘Tis the season and it tasted sooooo good.
I developed quite a nasty headache on the ride home and was very glad we didn’t live any further than the 60 miles away we already did. The second I got in the door I had a cold cloth ready, heated my beanbag neck wrap, and crawled into bed for a good 7 hours. All the while keeping a pillow over my groin area so the cats wouldn’t jump directly on it. They did very good….been there, done that and I think they knew mommy wasn’t feeling well and cuddled with me all night.
My sleeping and eating pattern is all out of whack now and my groin is still giving me some pain. I’m pretty tired and not real stable. My head is going back and forth on whether it wants to bother me or not, but nothing I can’t handle. I’ve been in worse pain, been in worse condition, and I’m just lucky to be here.
However, there still is that lingering “issue”. Blood has gotten back into my original brain aneurysm and it’s still sitting there. Dr. Ecker wants me to get an MRA so we have a really good baseline image as it stands right now, then we’re hoping to just have MRA’s next time and not have to go through an angiogram as frequently. I’m all for that. Not that I enjoy MRA’s, but it’s far less invasive than angiograms, just loud and annoying. Then if they notice a change on an MRA, another angiogram will be ordered for a closer look.
I came away from this angiogram with mixed feelings. Yes, it’s great news that things hadn’t changed from last year, BUT there is still blood sitting there in the neck of a brain aneurysm that has already ruptured and we haven’t really resolved what to do with that. It’s almost a deja vu of last year. Something I guess I’ll still worry about until we see otherwise one way or the other. I don’t feel like I’m out of the woods yet from that pesky 11mm brain aneurysm. I should give it a name…any suggestions? (Keep it clean!)